Can we halt memory loss as we get older?
It’s a fact of human life that we lose physical and mental function as we get older. In the information age that we currently live in, this translates into a decline in our ability to function and perform the activities of daily living. Can we halt or delay age-related memory loss?
 Min Wang and colleagues from Yale University School of Medicine in the August 11 issue of Nature, have published some elegant research that suggests we may be able to, at some point in the future.
Min Wang and colleagues from Yale University School of Medicine in the August 11 issue of Nature, have published some elegant research that suggests we may be able to, at some point in the future.
It’s important to distinguish the cognitive loss associated with normal ageing from that associated with dementias such as Alzheimer’s disease where major changes to the brain structure and function occur. The Yale researchers accomplished this by using aged monkeys that have a highly developed prefrontal cortex (PFC), the part of the brain associated with working memory. Monkeys, unlike humans, do not develop age-related dementias!
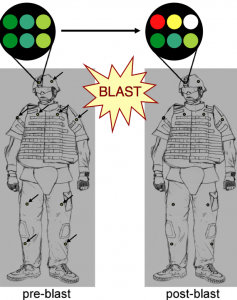
Working memory that allows you to keep things “in mind” e.g. where you put the car keys down, relies on a network of pyramidal neurons in the dorsolateral PFC that excite each other.
The strength of this excitatory network depends on the neurochemical environment e.g. elevated cAMP signaling reduces nerve firing. Wang and colleagues reversed the age-related decline in PFC activity by restoring an optimal neurochemical environment. Through a series of experiments they found that:
The memory-related firing of aged DELAY neurons was partially restored to more youthful levels by inhibiting cAMP signalling, or by blocking HCN or KCNQ channels.
These findings reveal the cellular basis of age-related cognitive decline in dorsolateral PFC, and demonstrate that physiological integrity can be rescued by addressing the molecular needs of PFC circuits.
This research, although preliminary and based on animal models, is promising. It offers the hope that in the future we may be able to reverse or slow-down the age-related memory loss and cognitive defects we would otherwise experience.
Many biotechnology and pharmaceutical companies are focusing on Alzheimer’s disease as a target. What this research suggests is that developing therapies that may delay or slow-down age-related memory decline could also be a valid target for drug development, with a significant market opportunity.
![]() Wang, M., Gamo, N., Yang, Y., Jin, L., Wang, X., Laubach, M., Mazer, J., Lee, D., & Arnsten, A. (2011). Neuronal basis of age-related working memory decline Nature, 476 (7359), 210-213 DOI: 10.1038/nature10243
Wang, M., Gamo, N., Yang, Y., Jin, L., Wang, X., Laubach, M., Mazer, J., Lee, D., & Arnsten, A. (2011). Neuronal basis of age-related working memory decline Nature, 476 (7359), 210-213 DOI: 10.1038/nature10243