Drug Discovery Targets Cancer Vulnerabilities

Miami Beach Lifeguard Tower
This week I’ve been at an American Association for Cancer Research (AACR) conference in Miami on “Targeting the Vulnerabilities of Cancer,” part of their Precision Medicine Series (Twitter #AACRpm16).
What’s interesting about AACR small specialist meetings is as well as listening to high quality talks, they create a relaxed atmosphere for networking and catching up with experts informally. The conference this week was relevant to anyone with an interest in cancer drug discovery.
 Although cancer immunotherapy remains the hottest topic in cancer drug development, we shouldn’t forget that there are other therapeutic targets worth exploring; several potential new opportunities were highlighted in Miami.
Although cancer immunotherapy remains the hottest topic in cancer drug development, we shouldn’t forget that there are other therapeutic targets worth exploring; several potential new opportunities were highlighted in Miami.
As readers know we don’t share unpublished data on the blog, so what I’ve done is provide a top-line summary of some of the strategic themes and key take homes I took from several of the presentations.
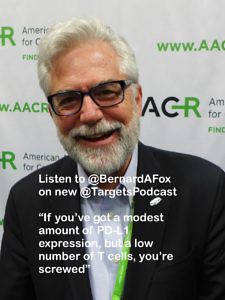
As an aside, If you haven’t already done so, do listen to the latest episode of the Novel Targets podcast – Of Mice and Men – it features excerpts of interviews recorded at the recent AACR annual meeting in New Orleans. I was surprised by some of what I heard!
For more information on forthcoming AACR meetings and workshops, check out the events calendar on the AACR website.
If you would like to read my commentary from the AACR Precision Medicine Conference in Miami on Targeting the Vulnerabilities of Cancer, subscribers can login below or you can purchase access.
This content is restricted to subscribers
 After exploring the science behind chemotherapy improving T cell trafficking into the tumour yesterday – which is one of the key rate limiting issues that need to be addressed with immunotherapies such as checkpoint blockade – some obvious follow-up questions comes to mind:
After exploring the science behind chemotherapy improving T cell trafficking into the tumour yesterday – which is one of the key rate limiting issues that need to be addressed with immunotherapies such as checkpoint blockade – some obvious follow-up questions comes to mind: A number of industry friends have uniformally expressed concern over how difficult it has been enroll such trials and bemoaned the broader – and often not anticipated – effect to the extent that some trials have even been terminated.
A number of industry friends have uniformally expressed concern over how difficult it has been enroll such trials and bemoaned the broader – and often not anticipated – effect to the extent that some trials have even been terminated. In the past, much of the focus at previous American Society of Hematology (ASH) meetings in this area has focused on the myriad of chemotherapy regimens and dose/schedule optimisations that followed in trying to boost patient outcomes.
In the past, much of the focus at previous American Society of Hematology (ASH) meetings in this area has focused on the myriad of chemotherapy regimens and dose/schedule optimisations that followed in trying to boost patient outcomes.