A potential new Immunotherapy in Breast and Ovarian Cancer
There has been a lot of negative publicity around Dendreon and sipuleucel-T (Provenge) recently, and the lack of a clear mechanism of action remains a concern to many.
Irrespective of the company’s commercial performance, sipuleucel-T remains an FDA approved therapeutic cancer vaccine that provides a benefit to some patients. It provided a proof-of-concept that immunotherapy can offer a survival advantage, albeit for a median of 4.1 months in asymptomatic advanced prostate cancer.
Dendreon is learning the hard way the failings in its commercial strategy, and no doubt these will be absorbed by others with other therapeutic vaccines in development.
Which brings me to an interesting paper published online first on November 8, 2011 in the American Association for Cancer Research journal, Clinical Cancer Research.
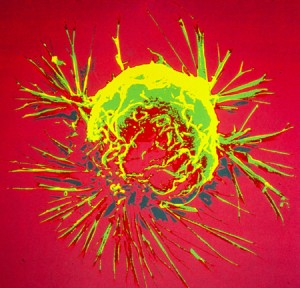
Researchers from the National Cancer Institute (NCI) published data from a small pilot trial showing a clinical response to a poxviral vaccine (PANVAC) in metastatic breast cancer and ovarian cancer patients.
Twenty six patients were in involved in the pilot NCI trial with PANVAC, a recombinant poxviral vaccine expressing the tumor-associated antigens (TAA), carcinoembryonic antigen (CEA) and mucin-1 (MUC-1).
The results showed a median overall survival of 13.7 months in the 12 breast cancer patients with four patients having stable disease, and one patient on study for 37 months. One patient had a 17% reduction in mediastinal mass.
In ovarian cancer, median overall survival for the 14 patients treated was 15.0 months.
This is promising early stage data in very sick patients. Mahsa Mohebtash and colleagues conclude in their paper that:
“Some patients who had limited tumor burden with minimal prior chemotherapy seemed to benefit from the vaccine. Further studies to confirm these results are warranted.”
Immunotherapy holds a lot of promise. Research suggests that cancer vaccines once they have provoked a response may improve a patients’ response to subsequent therapies through enhanced T-cell response.
The NCI researchers in their paper noted that time to progression and tumor shrinkage may not be good endpoints for evaluating immunotherapies given that it can take a few months for the optimal result after vaccination and there is often little impact on the tumor size, as judged by classical RECIST measurement.
Instead, overall survival (OS) should be considered a more relevant endpoint. Sipuleucel-T failed to show a benefit in progression free survival (PFS), but did show an impact on OS. In prostate cancer, OS remains the gold standard for regulatory approval, which is why Exelixis recently took a hit for not making this the primary endpoint in their phase III trial (306) for cabozantinib (XL184).
There are several challenges to consider with vaccine therapies:
- How do we identify upfront which patients are most likely to respond to the vaccine?
- The ideal setting is likely to be adjuvant rather than metastatic disease, but these trials will take a very long time and significant funding to come to fruition.
- Cancer vaccines may allow some patients to live longer, but they have yet to show any meaningful benefit in other clinical measures such as bone pain, symptoms etc.
- There are fewer side effects, but how do we evaluate how well patients are doing without clinically validated surrogate markers to aid in assessment?
This early research with a vaccine in breast and ovarian cancer, albeit on a very small number of patients, adds further support to the notion that vaccines may offer treatment benefits in the future.
We still, however, have a long way to go in understanding how best to use immunotherapy effectively and incorporate it into clinical treatment guidelines. We should also be wary of false hope and hype – I look forward to following the progress of PANVAC going forward.
![]() Mohebtash, M., Tsang, K., Madan, R., Huen, N., Poole, D., Jochems, C., Jones, J., Ferrara, T., Heery, C., Arlen, P., Steinberg, S., Pazdur, M., Rauckhorst, M., Jones, E., Dahut, W., Schlom, J., & Gulley, J. (2011). A Pilot Study of MUC-1/CEA/TRICOM Poxviral-Based Vaccine in Patients with Metastatic Breast and Ovarian Cancer Clinical Cancer Research, 17 (22), 7164-7173 DOI: 10.1158/1078-0432.CCR-11-0649
Mohebtash, M., Tsang, K., Madan, R., Huen, N., Poole, D., Jochems, C., Jones, J., Ferrara, T., Heery, C., Arlen, P., Steinberg, S., Pazdur, M., Rauckhorst, M., Jones, E., Dahut, W., Schlom, J., & Gulley, J. (2011). A Pilot Study of MUC-1/CEA/TRICOM Poxviral-Based Vaccine in Patients with Metastatic Breast and Ovarian Cancer Clinical Cancer Research, 17 (22), 7164-7173 DOI: 10.1158/1078-0432.CCR-11-0649