Following a death due to tumor lysis syndrome, AbbVie ($ABBV) have suspended the ABT-199 clinical trial program. ABT-199 is a promising new drug in development for chronic lymphocytic leukemia (CLL) that was about to enter phase 3 drug development by the company.
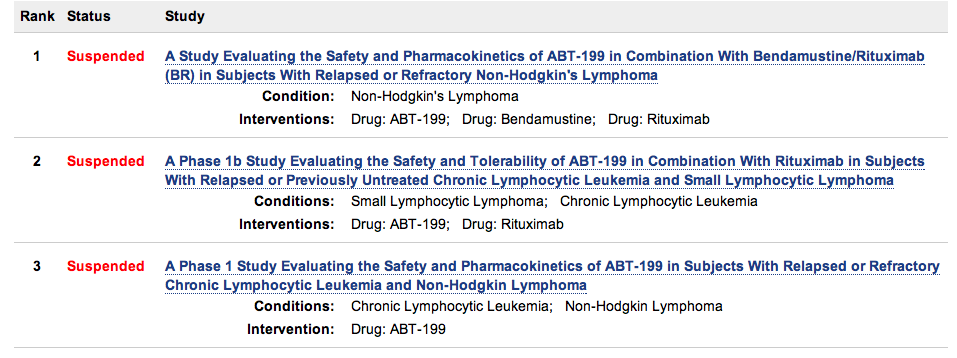
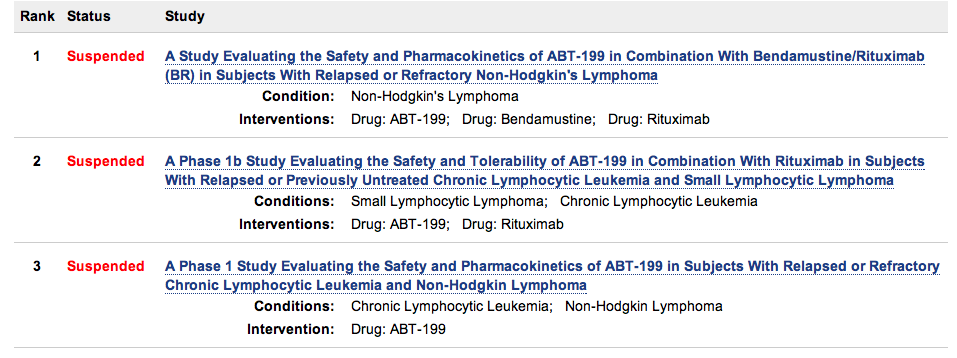
The company has issued no press release, but the clinicaltrials.gov web site shows that that clinical trials are suspended, information confirmed at the BIO CEO 2013 meeting in New York earlier this week. Here’s a quick snapshot taken on Feb 14, 2013 of what the clinicaltrials.gov site shows:
I first wrote about ABT-199 last year at the 2012 AACR annual meeting where Steven Elmore from Abbott (the predecessor of AbbVie) presented data showing it to be a new Bcl-2 inhibitor that overcame the side effects seen with navitoclax (ABT-263), which led to dose-dependent thrombocytopenia.
At the 2012 annual meeting of the American Society of Hematology in December, Matthew Davids, MD presented the results from the first-in-human phase 1 multicenter trial in patients with relapsed or refractory CLL and non-Hodgkin lymphoma (NHL).
Dr Davids declined to offer any comment on the suspension of the ABT-199 clinical trial program. By email he wrote, “I’m not able to discuss any data from the ABT-199 study that has not yet been publically presented.”
I thought this was a rather weak response given the fact the trial suspension is public knowledge. There’s more to being a thought leader than just being a company trial spokesperson who presents company prepared slides at scientific meetings.
It was also disappointing given the expertise at the Dana Farber Cancer Institute with BCL-2 antagonists, as evidenced by a recent publication on ABT-199 in the journal Cell by Dr Davids and Dr Letai earlier this week. Dr Letai previously wrote in the journal “Blood” that the “antagonizing function of Bcl-2 is an attractive goal in chronic lymphocytic leukemia (CLL) and other lymphoid malignancies.”
According to a reliable source, the ABT-199 clinical trial program has been suspended due to the trial participant dying from tumor lysis syndrome.
Tumor lysis syndrome (TLS) is a life-threatening cancer treatment complication where large number of cells die and deposit their contents into the blood stream. The kidneys and liver are overwhelmed trying to process and excrete the dumped intracellular contents. Acute renal failure may result. TLS is most common in fast growing cancers such as acute leukemias and less common in indolent disease such as lymphomas and CLL.
This last factor makes the issue for AbbVie and those medically supervising the trial more challenging in deciding whether the event was a one-off fluke or whether the TLS was drug related i.e. there is something in the way ABT-199 acts that poses a risk of TLS in the same way navitoclax caused dose-dependent thrombocytopenia. It could be related to dose-scheduling, for example, or the compound structure itself.
A patient death is something to be taken seriously, particularly in early stage development. Far better to find out you have a problem soon before spending multi-million dollars on a phase 3 drug development trial as AbbVie were poised to do.
Hematology industry expert Sally Church, PhD who writes Pharma Strategy Blog tells me that she thinks the ABT-199 clinical trials program will re-start, and sees this as a temporary setback once the dose-scheduling has been modified. Her view is that:
“There are risks associated with any new drug in development largely because so much is unknown. We don’t know what dose the patient was taking or for how long, but it’s possible that the agent is very effective and caused a much more rapid effect than expected at a high dose. They may need to be more cautious about the dosing going forward.”
ABT-199 if it makes it to market will compete against other promising new compounds in development for CLL such as ibrutinib, which received breakthrough designation from the FDA earlier this week.
Update Feb 15, 2013 AbbVie says they expect ABT-199 trials to continue but advise there are 2 patient deaths!
Thanks to Derek Lowe on “In the Pipeline” for picking up on the ABT-199 story this morning and for providing additional commentary and insight on tumor lysis syndrome.
His updated post this afternoon now includes a response from AbbVie, in which the company spokesperson confirms the voluntary suspension of the trials, that the problem is indeed tumor lysis syndrome and they expect dose escalation to control it.
They go on to say in their email that “we have every expectation that the clinical trials will come off hold and that we will be able to initiate Phase 3 trials as planned.” I encourage you to read Derek’s post if you have not already done so.
The fact there are 2 patient deaths from tumor lysis syndrome (I was only aware of one when I wrote this piece) now raises the question of whether the cause of this may indeed be related to the chemical structure of ABT-199. It’s clearly a serious matter that will at the very least delay AbbVie’s phase 3 drug development program for ABT-199.
Update Feb 18, 2013 Tumor Lysis Syndrome explained
Sally Church, PhD has published a post on Pharma Strategy Blog that is well worth reading: “Tumor Lysis Syndrome – what it is and why it is important in cancer research.”
In addition to commenting on ABT-199, Church discusses the potential for delayed Tumor lysis syndrome (TLS) seen with CTL019, the novel Novartis chimeric antigen receptor therapy (CART) in early stage development.
Update May 29, 2013 Clinical data on ABT-199 at ASCO 2013
In my pre-ASCO 2013 post on Chronic Lymphocytic Leukemia (CLL) that I published on May 28, 2013, I included commentary on ABT-199. Here’s the relevant excerpt:
At ASCO 2013 there will be updated phase 1 results for ABT-199 (GDC-0199) in CLL, and the main topic of discussion will be two clinical trial deaths that occurred due to tumor lysis syndrome.
At the recent 2013 AACR annual meeting, Rod Humerickhouse, MD, PhD from AbbVie Global Pharma R&D, said the company plans to start an ABT-199 phase 2 single agent study and a phase 3 combination study in CLL later in 2013/early 2014.
He told the AACR audience that Tumor Lysis Syndrome (TLS) adverse events occurred in 9 out of the 74 patients enrolled in three ABT-199 CLL clinical trials.
Two CLL trial participants died from TLS, and one had acute renal failure.
Notwithstanding the early promise of ABT-199 that I wrote about from the AACR 2012 and ASH 2012 annual meetings, these deaths have in my mind placed a substantial question mark over the safety of ABT-199, especially if other less-toxic therapies are available by the time it potentially comes to market. TLS is a sign of a highly effective drug, but whether dose modification can make it safe while maintaining efficacy remains to be seen. We don’t yet have the data to show this, and even assuming this data is forthcoming at the very least the development of ABT-199 has been set back in terms of time to market.
Whether the tragic deaths should have been avoided we may never know, there remain unanswered questions as to whether the dose escalation was too aggressive, whether the risk of TLS was known, and if so whether patients were properly monitored.
Relatives of both patients who died have sent in comments to the blog, highlighting the personal tragedy of losing a father or husband in this way. I can appreciate that after 33 years of marriage suddenly losing a husband at age 56 is pretty devastating, especially when the AbbVie company response appears to have fallen short in compassion and empathy:
“All I got was a quick phone call, after I left a message that he dropped dead in my bathroom, to thank me for letting them know of his passing and a condolence card.”
Although the development of ABT-199 looks set to continue, in my view it is no longer a front runner in the race to market in CLL. You can read more about the companies in the race to market in CLL in my pre-ASCO 2013 post.