Update on Orteronel TAK-700 from EAU 2012 Paris #EAU12
There are no major presentations of phase III clinical trial data at the European Association of Urology (EAU) Congress in Paris this weekend, but interesting clinical and scientific data is still being presented.
If you want to understand the competitive dynamics of the prostate cancer market and the market opportunity with urologists, then you need to be at meetings such as EAU in Europe and AUA in the United States.
There was a lot of interest in yesterday’s advanced prostate cancer poster session at EAU 2012.
I mentioned in a previous post that the radium-223/Alpharadin poster showed the data on skeletal-related events presented last month at ASCO GU in San Francisco.
Another poster that caught my attention for a variety of reasons was the one on orteronel (TAK-700), something that we have not heard too much about.
Activity and Safety of the Investigational Agent Orteronel in Men With Nonmetastatic Castration-resistant Prostate Cancer and Rising Prostate-specific Antigen: Results of a Phase 2 Study
Orteronel (TAK-700) is a selective, non-steroidal inhibitor of 17, 20 lyase, a key enzyme involved in the production of androgens such as testosterone. This is a similar mode of action to abiraterone acetate (Zytiga) that was approved last year in the US & Europe.
Orteronel is being developed by Millennium. Two phase III castration-resistant prostate cancer trials are currently enrolling. The post-chemotherapy trial (NCT01193257) is scheduled to have a primary completion date of September 2013 and the chemotherapy-naïve trial has a primary completion date of January 2013 (NCT01193244) according to clinicaltrials.gov at the time of writing.
It is worth noting that both phase III trials are using the drug in combination with prednisone. I doubt very much that the chemotherapy-naïve trial will show overall survival results by January 2013 (a date earlier than the post-chemo trial). This date must reflect when data on the primary outcome measure of radiographic progression free survival (rPFS) will be obtained.
Does rPFS correlate with overall survival? Many oncology new products have shown progression free survival, but no overall survival.
Is there a market for a “me too” of abiraterone? By the time orteronel comes to market, MDV3100 and Alpharadin will both most likely be approved, plus we will have greater insight into combinations and sequencing by then.
In talking to urologists, there is a clear preference for drugs such as MDV3100, which do not require the administration of concomitant steroids.
The phase II data in the poster presented at EAU yesterday concluded:
In patients with nmCRPC and rising PSA, single agent oral orteronel, at a dose of 300 mg BID without prednisone, was feasible and had manageable toxicities.
While it may be possible to administer orteronel without steroids, given the mechanism of action would it still be as effective? The authors also noted in the poster that 2 patients (out of 38) discontinued treatment due to adrenal insufficiency, suggesting that giving the drug without steroids is going to require active surveillance.
Finally, in thinking about TAK-700, I’m left with the question of whether phase III placebo controlled clinical trials are still ethical in advanced prostate cancer patients? In the post-docetaxel indication, we now have cabazitaxel and abiraterone approved, both of which offer an overall survival benefit. MDV3100 and Alpharadin are also expected to be approved by the FDA later this year.
If we have four new agents available after docetaxel that offer a survival advantage, is it ethical for men with advanced prostate cancer to be offered a placebo? If not, then this means that new products will have to go head-to-head with one of the approved drugs, or offer some additive effect if used in combination.
It will be interesting to see if this important issue is taken up by any of the patient advocacy groups and whether physicians start to raise concerns. Recruitment into placebo controlled trials could end up slower as a result.
Orteronel to me is too similar to abiraterone, which I think will face serious challenge from MDV3100. What the market opportunity for Millennium will be as a result of being late to market is an open question.

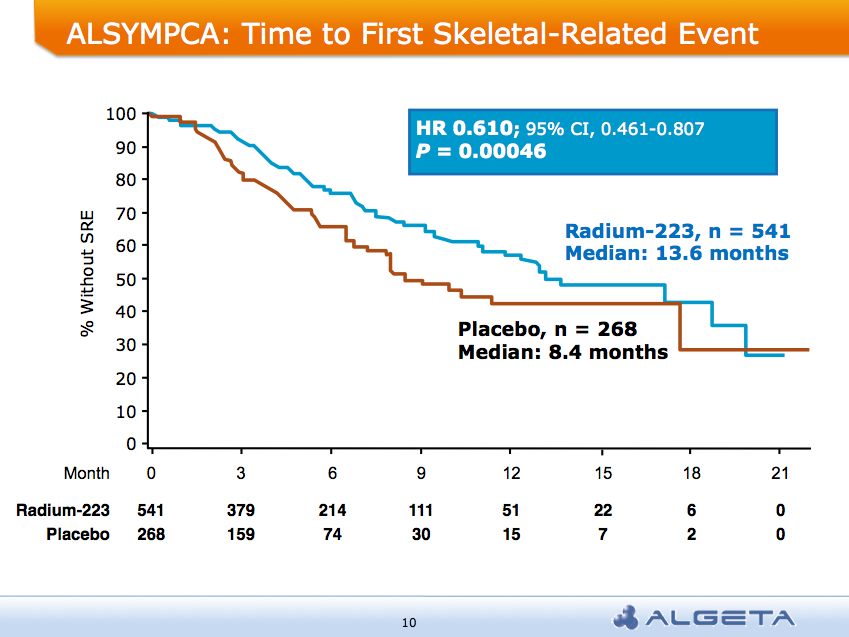 AND a median overall survival of 14 months compared to 11.2 months for placebo group:
AND a median overall survival of 14 months compared to 11.2 months for placebo group: