It’s been quite a roller coaster week so far for CAR T cell therapies, with Gilead announcing its intended acquisition of Kite Pharma on Monday. If that wasn’t enough, Wednesday brought another surprise – the FDA approved a rare double header – for Novartis’s CTL019, now known as tisagenlecleucel (Kymriah) for pediatric and young adult patients with a form of acute lymphoblastic leukemia (ALL), as well as a new indication for Genentech’s tocilizumab (Actemra) for the treatment of CAR T cell-induced severe or life-threatening cytokine release syndrome (CRS) in patients two years of age and older.
Inevitably there has been much hullabaloo and much anticipation over the expected price tag that might accompany the first cell therapy product approved in the US. Whatever your view on this, many of us were no doubt relieved it came in under $500K ($475K, with no charge for the product in the first month if there was a manufacturing failure or no response). While undoubtedly pricey, frankly it could have been a lot worse given the relatively small patient population.
Of course, the approved therapy isn’t the only expected high ticket item – there’s also hospital costs (including highly trained physicians and nurses), ICU costs (for very sick patients), supportive care costs (including tocilizumab if CRS occurs), not to mention any lab, diagnostic or monitoring tests required. All of these will no doubt push the total bill nearer to $1M. In children though, the lifetime value of curative intent and many additional years of life is a much easier to grasp concept for payers than adding a few extra months at a high cost in adults.
These issues do raise the stakes for Kite and what they plan to do strategically in aggressive lymphomas, where there is a larger pool of eligible people for therapy, which must be offset by lower response rates (vs. pALL) and likely lower durability based on the data we’ve seen to date. If we are truly moving into a world of value based pricing in the US, then efficacy and tolerability will ultimately have an impact on the perceived cost and value of treatment.
As Warren Buffett, the famous value investor has been want to say, “Price is what you pay, value is what you get.”
Whoa that’s a lot to think about – who knows what Friday may bring at this rate – and we still have the Kite Axi-Cel approval in aggressive lymphomas to go yet…
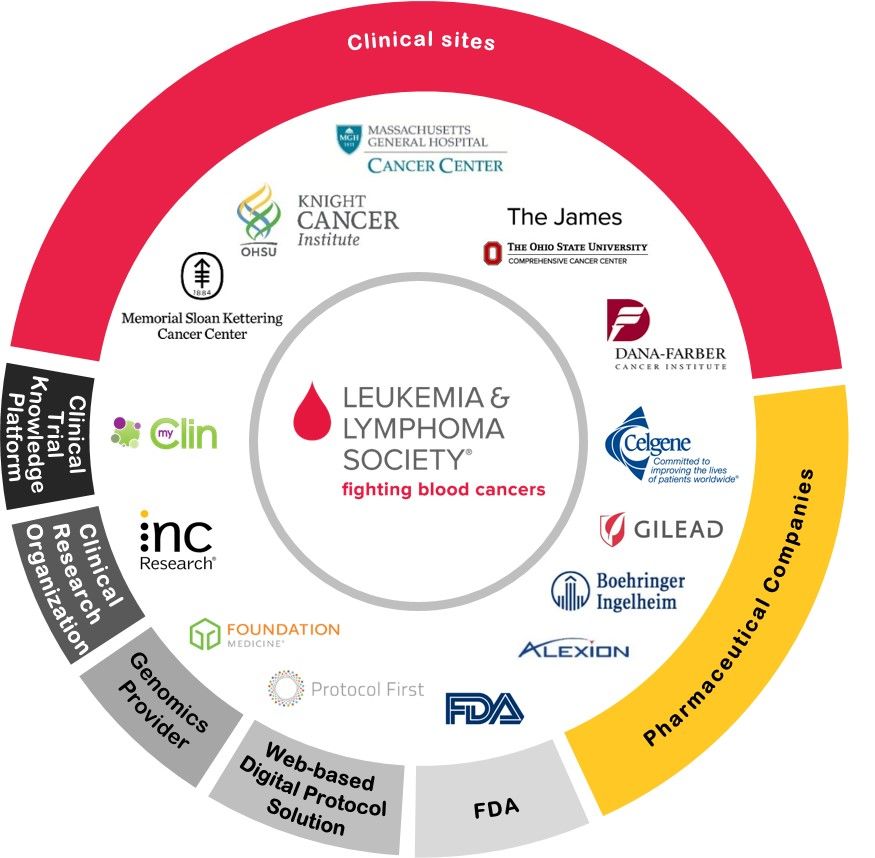
Meanwhile, there’s also a high unmet medical need for new effective treatment options in Acute Myeloid Leukemia (AML), especially in the relapsed/refractory setting, which is why we’re firm supporters of the Beat AML trial that the Leukemia and Lymphoma Society are pioneering. (See: Interview with Dr Brian Druker).
There’s also interest from several companies in a variety of novel targets, including CD123.

Notre Dame, Paris
Cellectis recently announced the enrollment of the first AML patient into their trial of an allogeneic CAR T cell therapy (UCART123) targeting CD123.
Quite aside from the issue of addressing whether such a product can be administered safely and effectively, one major why there is notable interest in Cellectis is because an allogeneic CAR T cell therapy offers the potential of a much cheaper off-the-shelf product as well as enhanced performance from an abundance of fit immune cells from healthy donors rather than tired or exhausted ones from people who are sick, thereby reducing the risk of manufacturing failure.
While in Paris, I spoke with Cellectis Chief Medical Officer, Loan Hoang-Sayag, MD about the trial design and CD123 as a target in AML.
This is the third and final post in our summer mini-series on gene editing and allogeneic CAR T cell therapy.
The first in the series featured an interview with Professor Waseem Qasim (Link), and the second with Cellectis CSO, Dr Philippe Duchateau (Link).
To learn more insights on this intriguing topic, subscribers can log-in or you can gain access to BSB Premium Content.
This content is restricted to subscribers
 One of the big challenges with cancer research is sorting out the wheat from the chaff in terms of viable targets.
One of the big challenges with cancer research is sorting out the wheat from the chaff in terms of viable targets.
 As part of our #JPM18 coverage we like to feature up and coming companies to watch out for, one of these is Syros Pharmaceuticals (NASDAQ: SYRS). In this post we take a look at what’s on the horizon for the company in 2018?
As part of our #JPM18 coverage we like to feature up and coming companies to watch out for, one of these is Syros Pharmaceuticals (NASDAQ: SYRS). In this post we take a look at what’s on the horizon for the company in 2018?



 As Dr Mario Sznol (Yale)
As Dr Mario Sznol (Yale)