ASH 2013 Preview – Chronic Lymphocytic Leukemia (CLL)
The chronic lymphocytic leukemia (CLL) landscape has been one of the most dynamic and exciting over the last 12 months, with many new therapies emerging against different targets from CD20 to BCR signaling, Bcl2 to the PI3K pathway. Other new targets may also soon emerge.
The annual meeting of the American Society of Hematology (ASH) in New Orleans sets the scene for the rollout of more mature data and affords an early evaluation of where the various companies competing in this space may shake out. Given that we are moving beyond traditional chemoimmunotherapy to evaluate several newer classes of therapy including B cell receptor (BCR) and PI3K signaling, anti-CD20 antibodies, anti-CD19 chimeric antigen receptor T cell technology (CART) it looks to be shaking out to an exciting conference.
Companies mentioned: Roche/Genentech, Gilead, Pharmacyclics, Abbott, Celgene, Infinity, Incyte, ONO, Amgen, TG Therapeutics, Novartis
Products discussed: rituximab, bendamustine, obinutuzumab, idelalisib, ibrutinib, ABT-199, CC-292, GS-9973, IPI-145, ONO-4059, INCB40093, AMG 319, TGR-1202, CTL-019
This content is restricted to subscribers
1. German CLL10 trial – FCR vs BR in frontline CLL
This content is restricted to subscribers
It might surprise many readers to learn that this is one of most highly anticipated trial results from ASH given that it looks at old style chemoimmunotherapy. This is a large phase III study run by the German trial group. It seeks to answer the question of which is the better option upfront – chemoimmunotherapy with FCR or a doublet with bendamustine plus rituximab?
For most practising hematologists on both sides of the pond, this has been an eagerly awaited study.
With 547 patients evaluable for response and 561 for PFS analysis, this interim analysis from a large head to head trial could potentially afford an opportunity to decide optimal front-line treatment for patients with good performance status and potentially determine the optimal standard of care.
You can check out the detailed abstract here.
Let’s take a look at the data. At first sight, the analysis looks in favour of FCR from an efficacy perspective, especially in the depth of response:
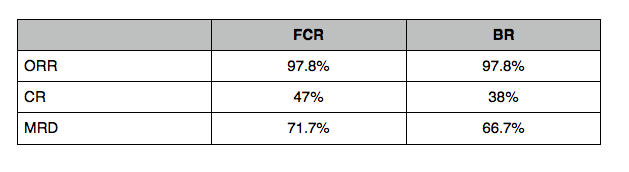
Where MRD is an indication of minimal residual disease – the higher the number, the better. Notice the high degree of CRs achieved in either arm.
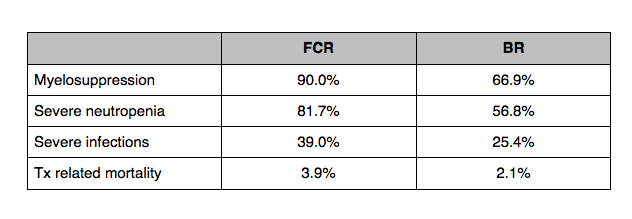
The groups were also balanced for number of cycles and thus each arm received similar treatment exposure. The side effect profile clearly favoured the BR arm – the improved efficacy with FCR comes with a price:
There are a couple of other important points to note. While the abstract suggests that the groups were balanced for age, stage of disease, 11q mutation status etc, there is one critical caveat:
“There were significantly more patients with unmutated IGVH in the BR arm (68%) in comparison to the FCR arm (55%; p=0.003).”
Ah… so this means that more patients in the BR arm had an unmutated BCR signaling pathway, which gives a worse prognosis. The efficacy difference in favour of FCR could therefore be easily explained by the unfortunate imbalance.
This glaring mistake is surprising for such an elite study group and may well be why the authors were forced to conclude that:
“In light of these results, no firm recommendation of one regimen over the other can be given at the present time regarding the first-line use in CLL patients with good physical fitness.”
2. Obinutuzumab/Gazyva (Roche/Genentech)
As predicted earlier this year, the plenary session at this year’s ASH includes a presentation on the frontline phase III trial in CLL patients ineligible for chemotherapy due to co-morbidities (German CLL11).
Recall that this was a two-part randomized study, the first part compared the doublets of chlorambucil plus either rituximab or obinutuzumab to chlorambucil alone and was highlighted at ASCO.
The second part, which is the focus at ASH, is a head to head comparison of rituximab plus chlorambucil vs obinutuzumab plus chlorambucil. Roche have already confirmed that the study met its primary endpoint of PFS (26 vs 15 months in favour of the obinutuzumab arm), so we do know that the second generation anti-CD20 monoclonal is far superior – almost a year of extra life before their disease worsens is huge for patients, even those with indolent disease.
What many people do not realise is that over time, we may see the overall survival curves pushed out by a noticeable amount with sequencing of a multitude of new therapy combinations. This particular combination provides a solid combination from which to build from in the elderly population.
For those wishing to learn more about the background to the study and how obinutuzumab is different from rituximab, you can check out the following articles:
a) Background on obinutuzumab and glyco-engineering (guest article on C&EN)
b) An interview with Dr Susan O’Brien on the emerging CLL landscape
At ASCO, there were some initial concerns about the higher infusions reactions seen with obinutuzumab, but KOLs I spoke to who were involved with the study said that they tended to occur on the first infusion, were manageable with appropriate supportive care and subsequently disappeared. I think had they persisted throughout the treatment cycles, it would have been a much bigger concern.
Strategically, you can see where Roche/Genentech are going with their compounds in CLL and NHL and why I’m so excited about the potential for combining obinutuzumab with GDC-0199 in this recent interview with one of their scientists.
3. Idelalisib (GILD from Calistoga)
This PI3K-delta inhibitor was formerly known as CAL-101 and many of us will no doubt continue to think of it that way, as it’s one of those catchy code names that tend to stick!
a) Can idelalisib be safely combined with rituximab?
Recall the interim trial results from the frontline trial were presented at ASCO by Susan O’Brien. But what happens in the relapsed/refractory setting? The rationale for the combination is a logical one, given that it targets two key elements of the signaling associated with CLL.
The short answer appears to be yes based on this encouraging phase III study in heavily pretreated RR CLL, which is being presented in the Late Breakers on Tues am:
“At 24 wks, the PFS rate for IDELA + R was 93% compared to 46% for placebo + R. PFS strongly favored IDELA + R in all subgroups, including those with del(17p)/TP53 or unmutated IGHV.”
We don’t know the breakdown for the ORR by CRs and PRs yet, but the KM curves are clearly significantly in favour of the idelalisib arm.
Serious adverse events were consistent from previous studies and within expectations for the therapies involved:
“The most common SAEs were pneumonia (6.4%), pyrexia (6.4%), and febrile neutropenia (4.5%) in IDELA + R, and pneumonia (8.4%), febrile neutropenia (5.6%), and dyspnea (3.7%) in placebo + R.”
Given the oral CLL session is also on Tues am at the same time, I’m fervently hoping this one is later in the Late Breaker session and that the rooms are not too far apart!
b) Are there any differences when combining idelalisib with rituximab or ofatumumab?
This abstract is a poster based on a multi-center phase I study in the US in RR CLL (n=40). The combined efficacy data is given:
“The ORR (N=40) was 83% (33/40), with 3 CRs (8%), and a median (range) time to response of 1.9 (1.7‑21.8) months”
although I would be interested to learn if there are any differences between the two anti-CD20 antibodies in terms of efficacy and safety when idelalisib is added. A slightly lower, but still encouraging, response rate (73%) was reported in high risk patients.
c) Comparison of idelalisib with BR or chlorambucil
This phase I trial (n=29) evaluated combinations in RR CLL and found both to be tolerable. The efficacy data at the cutoff showed an ORR of 89.7%. It will be most interesting to see if the two arms differ because refractory patients tend to be:
- older
- have a poorer performance status
- bulky adenopathy
- are often worn out from years of continuous treatment.
This makes them a difficult group to evaluate, since AEs can be more challenging for them to tolerate over time.
Median PFS and DOR were not reached at the cutoff, but I look forward to seeing the KM curves in the poster. No overlapping toxicities were reported in the abstract, a good sign.
d) Can idelalisib have a positive impact in high risk patients?
Aside from the challenge of heavily pre-treated patients, another group that has an unmet medical need is high risk patients, who sadly do poorly on chemoimmunotherapy.
Steve Coutre and colleagues explored this subgroup in three phase I/II trials and included patients (newly diagnosed and RR CLL) with 17p and 11q deletions, TP53 mutations and the NOTCH1 mutation.
Clearly, one would expect to see more CRs in previously untreated than RR disease, but what about responses in the different aberrations? The efficacy responses are solid as shown in their table below:
What these results suggest is that high risk patients can be considered for idelalisib therapy rather than excluded given the response rates. What we don’t yet know are the durability of the responses, however, the number of CRs in the previously untreated patients is very encouraging indeed.
The big question many people have is which combinations are likely to work best with idelalisib in CLL?
Obviously, rituximab, ofatumumab, fludarabine, bendamustine and chlorambucil are logical partners. Such a trial is already ongoing (phase I) http://clinicaltrials.gov/ct2/show/NCT01088048 and may read out in time for next year’s ASH, but in the meantime, we have much new data to look forward to discussing next week.
4. Ibrutinib/Imbruvica (PCYC/J&J)
Even if one overlooks the Wall Street penchant for hype and enthusiasm, especially for stretched forecast expectations, the ibrutinib story in B cell receptor (BCR) signaling continues in a strong fashion. This is despite relatively low rates of CRs in the trials reported to date compared to standard chemoimmunotherapy doublets and triplets (see above).
Recently, FDA approved ibrutinib (Imbruvica) for MCL under the breakthrough designation, but at the time of writing, the RR indications in either CLL or SLL have yet to be announced. Hopefully, they will emerge soon given Priority Review status and an NDA filing date of June 28th.
So what does the latest data on ibrutinib in CLL from New Orleans offer?
a) Single agent therapy offers long term safety and durability
Susan O’Brien and colleagues report on two different subsets of CLL/SLL patients in this study – chemo naive and relapsed/refractory.The median time of therapy was almost 27 months upfront and 21 months in the advanced setting, where the median number of prior therapies was three.
One thing that caught my eye was the tolerability profile:
“The percentage of patients who had a grade 3 or higher serious adverse event (SAE) declined over time from 43% within the first year of study treatment to 32% after the first year of treatment.”
Drug related AEs also declined:
“The number of grade 3 AEs and SAEs also declined from within the first year of treatment (24% and 8%, respectively) to after the first year of treatment (7% and 0%, respectively).”
When you see side effects decline like this, that’s usually a good sign for a therapy taken chronically.
We will find out more about how the efficacy is doing in these groups at Ash but an encouraging mention was made that:
“At landmark 30 months, 76.1% of the responders were alive without progression.”
This is a good result. Based on what we know to date, it seems that targeting BTK with ibrutinib allows the disease to be kept in check and live longer, but without inducing a significant number of remissions.
b) Impact on patients with 17p deletions
This is an important subset of patients to explore because standard chemoimmunotherapy has little or no positive impact on their prognosis. In fact, they actually tend to do more poorly. The question then, is does targeting BTK help in this respect?
A phase II investigator study run by researchers from the NIH seeks to explore this issue in 53 elderly patients with and without 17p deletions. They report data from a median follow up of just over a year.
Interestingly, there were no differences between the groups in terms of the degree of disease reduction. Although the number of PRs was greater in the normal vs del17p group (81% vs 53%), the latter did better than one might expect overall. This was rather encouraging, I thought.
c) What happens when you combine ibrutinib with rituximab?
MD Anderson are presenting data from a single institution phase II study (n=40) with a follow up of approx. one year in high risk (del17p or TP53 mutation) patients with RR CLL. They posed the question of whether the combination leads to a better response rate (currently 71% as a single agent in RR CLL) in high risk disease?
Patients received the standard dose of ibrutinib (420mg PO QD) and rituximab (375 mg/m2) was administered weekly for the first four weeks (cycle 1), then monthly until cycle 6. Patients then continued on ibrutinib monotherapy.
The results so far suggest that the combination is safe and well tolerated, with good depth of response.
Only 2 grade 3 AEs are mentioned in the abstract – mucositits and peripheral neuropathy. However, of the 8 patients that came off study, 3 patient died from unrelated infectious complications (2 cases of sepsis, 1 case of pneumonia), another died from unrelated respiratory and cardiovascular failure. Two patients discontinued due to ibrutinib-related toxicity, namely a subdural hematoma and another experienced grade 3 mucositis.
To put these results in context, it should be noted that CLL patients are also prone to infections and related complications due to the nature of the disease.
The efficacy results look stronger in the combination than for historical monotherapy, although ideally this should be evaluated in a comparative study:
- PR 87%
- CR 8%*
- ORR 95%
Note: One CR was negative for MRD by flow cytometry.
ORR in patients with del17p or TP53 mutation (n=20) was 90% (16 PR, 2 CR), which is quite impressive. The big question, though, is how durable will these responses be? No doubt we will learn more at ASH.
One of the things I liked about this abstract was the chart showing the lymphocyte count over time. Recall that CLL is lymphocytic not myeloid leukemia, meaning that the lymphocyte count is very high in these patients, leading to severely swollen lymph nodes (known as bulky disease). This means that any therapy that can reduce the lymphocyte burden significantly will have a large impact on a patient’s quality of life.
To date, ibrutinib as a single agent hasn’t been shown to address the lymphocyte burden particularly well in high risk patients and in fact, Byrd et al., previously demonstrated that it can initially induce transient treatment related lymphocytosis in 78% of advanced CLL patients. However, the authors in this study observed some encouraging signs:
“Compared to ibrutinib monotherapy, the redistribution lymphocytosis resolves more rapidly and completely, and consequently the ORR is higher.”
Based on these encouraging results, I think we may well see a lot of interest from hematologists in the IR regimen, especially for advanced patients, the majority of who tend to have bulky disease.
d) Can ibrutinib be combined with BR in CLL effectively?
Bendamustine plus rituximab (BR) is a popular combination for CLL patients in the relapsed/refractory setting and is generally more tolerable than FCR (usually given upfront) in patients with a good performance status.
This multi-centre phase IB study (n=30) included high risk RR CLL patients with del17p (23%) and del11q (43%), as well as those with normal karyotype. They received up to 6 cycles of BR with a continuous fixed ibrutinib dose of 420 mg/day; ibrutinib dosing continued past 6 cycles until disease progression or other reason for discontinuation.
Frequently observed treatment-emergent AEs included GI events and myelosuppression:
- Diarrhea (70%)
- Nausea (66.7%)
- Fatigue (46.7%)
- Neutropenia (40%)
- Upper respiratory tract infection (36.7%)
Grade 3 or higher treatment‑emergent AEs were neutropenia (40.0%), maculopapular rash and fatigue (10.0% each), and thrombocytopenia, febrile neutropenia, and cellulitis (6.7% each).
The efficacy results from this triple combination were as follows:
- ORR was 93% (28/30 patients, including 5 CRs and 3 nPRs)
- One additional patient achieved a PR with lymphocytosis.
- The estimated 12 month PFS was 90%.
Given that the early results for IR and IBR appear to offer a similar high ORR, it remains to be seen whether including bendamustine in the combination adds significant efficacy without additional toxicities – a true head to head comparison trial in multiple centers would be an interesting study to evaluate. That said, a phase III trial evaluating BR with and without ibrutinib is already ongoing. http://clinicaltrials.gov/ct2/show/NCT01611090
In future, we may see similar combinations evolve with obinutuzumab rather than rituximab, but time will tell what happens on this front.
5. ABT-199/GDC-0199 (AbbVie/Roche)
This Bcl2 inhibitor targets the apoptosis pathway and induces cell death. Data from a phase I trial will be available. Recall that after the interim data last ASH, several patients with bulky disease received high dose escalations and unfortunately experienced TLS and died. While TLS can be a good sign that the drug is working, if the cytokine release is too rapid, it can be difficult for the body to excrete the cells being produced in massive numbers.
Hopefully, dose reductions and a slow escalation will have avoided the catastrophic events seen earlier this year. The abstract suggests encouraging signs are now emerging:
“ABT-199 showed activity in patients with R/R CLL with a response rate of 84% for the study population, including 20% CR/CRi. Patientss with high-risk CLL showed similar efficacy with a response rate of 82% in del(17p) and 78% in F-refractory disease.”
Where F is fludarabine, usually given upfront as FCR or FR to patients with a good performance status.
Once a safe and effective dose is found, it would make scientific sense to look at rational combination trials. Several are already ongoing evaluating ABT-199/GDC-0199 with rituximab and obinutuzumab to evaluate the pharmacokinetics.
It will not be a surprise to see more studies open to evaluate safety and efficacy further. I think this is one area where we will see more combinations evolve, such as combining Bcl2 and BTK inhibition given that Roche have a BTK small molecule in development.
6. GS-9973 (Gilead)
This compound targets Spleen tyrosine kinase (SYK), another element of the BCR signaling pathway that also includes BTK.
A little bit of history here. Several years ago at ASCO, the phase II data for Rigel’s SYK inhibitor caused quite a stir in the CLL community with impressive responses for Rigel’s inhibitor fostamatinib. I remember sitting in the media briefing at the time and thinking Wow!
Unfortunately, they partnered with AstraZeneca and decided not to proceed with the much anticipated phase III trial in CLL, choosing to pursue the much larger and potentially more lucrative rheumatoid arthritis (RA) indication instead. Sadly, that approach failed and the CLL indication never seems to have got off the ground. Strangely had the companies focused on CLL and the results urned out positively, they may well have beaten Pharmacyclics and their related BTK inhibitor ibrutinib to market, such is the quirkiness of R&D fortunes!
Fast forward to 2013 and we have a new SYK in development from Gilead. I first saw the PK and PD data from healthy volunteers at AACR earlier this year in combination with idelalisib, so it comes as no surprise that this compound is being evaluated in the clinic in patients.
Jeff Sharman and colleagues are presenting a poster on CLL or NHL (n=40 per group) treated with single agent GS-9973 800mg BID. The CLL cohort include high risk patients with del17p and TP53 mutations, all of whom had received prior anti-CD20 therapy. The initial AE readout suggests that fatigue, ALT elevation and GI issues such as nausea and diarrhea are the most common effects. I’m looking forward to seeing the data from this study, especially the chemokine and cytokine data and the updated efficacy results on a larger number of CLL/SLL patients.
If the results look as promising as expected, then I don’t think it will be long before we see a combination trial from Gilead exploring whether dual targeting of the BCR and PI3K signaling pathways is more effective than either alone. The general expectation is that this approach should lead to better long term survival, but we shall have to wait and see.
Should this approach be successful, then Gilead will be very well placed in CLL and NHL going forward.
7. IPI-145 (Infinity from Intellikine)
It was interesting to catch the gasps from the oncologists around me at ASCO when Infinity presented their data on IPI-145 in June – the increased infection rate was not well received and many wondered whether a dual delta gamma PI3K inhibitor would be a good thing, despite the hints of increased efficacy (55%) over Gilead’s idelalisib (~40%). Positioning this product is going to be an interesting challenge should the drug make it to market.
At ASH, Ian Flinn and colleagues are presenting the updated phase I study results. Efficacy appears to be in the same ballpark (52-53%), but still lower than ibrutinib monotherapy (~70%). However, unlike ibrutinib, there is no redistribution of lymphocytosis seen and reductions in adenopathy are noted, both good things. It is now clear that targeting different aberrations results in a different side effect profile.
The bad rap on the SAEs remain though:
“The most frequently-occurring SAEs were respiratory and/or infectious events occurring in 11 (25%) patients.”
I suspect though, that this can be managed in future clinical trials with anti-infective prophylaxis therapy to minimise the effect.
The good news is that they do have a RP2D:
“The PK/PD and clinical activity suggest that 25 mg BID is a biologically active dose in R/R CLL, and this dose has been selected for an upcoming randomized Phase 3 trial in R/R CLL.”
Whilst there has been quite a lot of handwringing over the efficacy:tolerability profiles of the selective PI3K inhibitors, I like the approach very much and believe that they will make a nice foundation for combination trials in CLL and NHL across different lines of therapy, which may lead to less resistance and better long term survival. The more immediate question for Infinity, though, is can they differentiate themselves from idelalisib? By that, they will need to demonstrate either superior efficacy or better tolerability. The count is still out on that one – positioning will be critical as the second to market agent in this class.
There are also other selective PI3K inhibitors in preclinical and clinical development, including Gilead’s second generation inhibitor, GS-9820, Incyte’s INCB40093, TG Therapeutics TGR-1202 and Amgen’s AMG 319, although some of these are fairly new developments, you can clearly see that others have languished during trial enrollment for quite a while.
8. CC-292 (Celgene from Avila)
Like many people, I was rather excited when Avila Therapeutics first announced their BTK inhibitor but sadly, since it was acquired by Celgene, the pace of development seems to have slowed down.
Phase I data is being presented at ASH in RR CLL/SLL (n=83). This dose finding trial explores 4 different doses/schedules including once and twice daily regimens. The sample sizes are a little small in two of the arms so it is hard to extrapolate too much. That said, the ORR ranges from 55-67% and PRs from 31-67%. Nodal responses were reported in two of the arms (23-24%), including those with high risk factors. It’s too early to draw conclusions here, but at first glance, the data looks to be less impressive than ibrutinib monotherapy.
A more detailed update will follow once I’ve seen the actual poster at the meeting.
9. ONO-4059
Ono Pharma are developing a BTK inhibitor, ONO-4059, in B cell malignancies. They have some interesting preclinical data at ASH that shows a combination of the BTK inhibitor with obinutuzumab has greater efficacy in vivo than the BTK inhibitor alone.
Early phase I data in RR CLL is also available (n=16) including high risk patients. It’s too soon to see how this agent will stack up to ibrutinib and CC-292, but the reduction in lymphadenopathy in heavily pre-treated patients with bulky disease is an indication that it has some clinical effectiveness. Since no DLTs have been reported yet, the MTD may not have been reached. This abstract has been selected as an oral presentation, a good sign as there are few of these at ASH to go around.
Finally, last but by no means least is an update on the Novartis CART program in CLL.
10. CTL-019 (Novartis/U. Penn)
After hearing Carl June’s lengthy (30 min) presentation at the recent AACR Molecular Targets meeting in Boston, I was rather looking forward to the updated clinical data at ASH in CLL, in particular. However, the first abstract on the subject left me feeling a little underwhelmed:
“As of 7/15/2013, 27 patients have been enrolled; T cells did not adequately expand in 3, 1 patient was not eligible after screening, and 10 patients have been treated.”
I’m therefore hoping this is merely a placeholder and that more substantial data will be presented in the Tues morning oral session! There was some encouraging news in that:
“4 of the first 10 patients treated have responded within 3 months.”
So we know that the responses can be rapid, but durability remains an unanswered question.
This question may be addressed in part by a presentation from Michael Kalos and colleagues from U Penn and Novartis look at the clinical responses in RR CCL and ALL in a separate oral session on Sunday in CD19 positive patients.
This abstract looks a little more encouraging:
“The initial cohort of patients is now disease free between 1 and 3 years post-infusion.”
Persistency and MRD data will be discussed from the original cohort, together with more recently treated patients.
What does this all mean?
If we consider the five main categories, namely anti-CD20, anti-CD19, BCR signaling (BTK and SYK), apoptosis (Bcl2) and selective PI3K inhibitors, it is clear that in future it may be possible to select patients for appropriate treatment in different ways other than the catch-all approach of chemo-immunotherapy with FCR, FR or BR.
While the monotherapy data is still shaking out across the board, I do think we will see more new novel combinations begin to evolve that both spare the ravaging effects of the chemotherapy of the past and also induce better cell killing effects. After all, what we all want to see is more durable CRs and MRD, which essentially can lead to longer lasting remissions.
Ibrutinib has been the fascination for many of late, but dual combinations such as idelalisib with a SYK inhibitor or obinutuzumab with ABT-199 may demonstrate greater efficacy than monotherapy in the long run. If that’s the case, then Roche and Gilead will be well placed given their ability to do combination trials. The big question remains how CART will stack up to all-comers because it’s potential to induce lasting MRD and remission is an attractive proposition.
Either way, the CLL landscape is changing and in 5 years time may be very different from the emerging trends we see now.
More detailed analysis will be posted from New Orleans each day as the presentations roll out.