Why don’t we have evidence based medicine for robot-assisted radical prostatectomy?
That was the question that I asked Walter Artibani, Professor and Chair of Urology at the University of Verona during the recent European Association of Urology (EAU) annual Congress in Paris.
Urologists have failed as scientists to generate evidence based medicine
Professor Artibani told the assembled media that urologists had failed as scientists in not generating robust clinical data to support the use of the da Vinci robotic system for the removal of the prostate gland (prostatectomy).
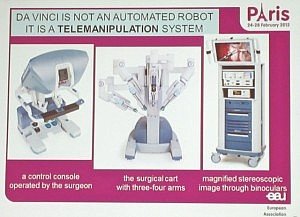 Something that I was not aware of until I attended the media briefing was that so called “robotic surgery” is not an automated robot performing the surgery on its own, but instead it’s actually robot assisted surgery.
Something that I was not aware of until I attended the media briefing was that so called “robotic surgery” is not an automated robot performing the surgery on its own, but instead it’s actually robot assisted surgery.
The da Vinci surgical device (currently the only one on the market) is a telemanipulation system where the surgeon sits at a remote console and operates a surgical cart with three or four arms that are docked with endoscopic instruments that are inserted into the patient.
Professor Artibani in response to my question said:
“After 10 years, the urologic community missed the window to have prospective randomized clinical trial in order to have clear answers.”
What’s more he went on to say that he believed it would be unlikely we could now do a prospective trial that compared robot-assisted prostatectomy to laparascopic prostatectomy to open prostatectomy. The reason for this was that :
“Most of the patients are convinced that the new way, the novel way is the better way.”
The following is a video excerpt of Professor Artibani’s answer to my questions. For digital accuracy, viewers should note that I added in some slides he presented earlier, and included a graphic of the paper he referenced.
http://youtu.be/jXImeY-f9j0
Have the media sensationalized robotic surgery?
Artibani went on to say in his answer to my question that the media and journalists have not always reported the lack of robust data surrounding new surgical techniques:
“It is easy just to give the information that what is new is better and this must be demonstrated by robust data before giving the information. Unfortunately sensationalism is more important than to say and to write robust data.”
Healthcare journalists have an obligation to report on the limitations of new techniques and lack of evidence based medicine is an important one! Gary Schwitzer’s healthcare journalist watchdog, Health News Review, attempts to hold the media to account.
We should clearly challenge surgical practice for which there is a lack of robust clinical data or evidence based medicine, and avoid sensationalism.
However, whatever the limitations of the media reporting, the reason for the lack of evidence based medicine rests firmly with the academic urology community.
Low quality of evidence for Robot-Assisted Laparoscopic Prostatectomy
In an editorial in the journal “European Urology,” Markus Graefen noted the low quality of urology research that was being published did not just apply to robot-assisted prostatectomy. He noted that in urology,
“The number of low-quality papers is increasing; however, the body of evidence and the knowledge we have about the reported outcomes, unfortunately, is not.”
He went on to describe the need to counsel patients on the different surgical approaches available to them:
A patient with a newly diagnosed prostate cancer who is counselled for his therapeutic options today should be informed that several equal surgical approaches are available and that despite all the perfectly styled Web pages, it is not the robot that makes the difference.
He should be informed that there are indeed concerns about oncologic and functional outcomes and also evidence that in some significant papers the traditional surgical approaches look superior.
This editorial suggests that patients should ignore the marketing hype about new equipment or the notion that “new is better,” but instead focus on the experience of the surgeon with that equipment and the functional outcomes that a surgeon obtains in his/her patients.
Patients are interested in functional outcomes and low complication rates
What I heard at EAU from urologists is that patients are interested in a good functional outcome and low complication rate.
There is, however, no level 1 evidence that post-operative urinary incontinence and erectile dysfunction rates are generally better with robot-assisted radical prostatectomy.
Diana Kang and colleagues in a review of seventy-five research publications between 2005 and 2008 that reported robot-assisted laparscopic prostatectomy (RALP) data, concluded that there was a need to raise the standards of urology clinical research:
Our findings draw into question to what extent valid conclusions about the relative superiority or equivalence of RALP to other surgical approaches can be drawn and whether published outcomes can be generalised to the broader community.
There is an urgent need to raise the methodologic standards for clinical research on new urologic procedures and devices.
Men with prostate cancer who are considering surgery should be informed that there is no high-level or robust evidence to show the general superiority of robotic-assisted prostatectomy compared to other surgical techniques for radical prostatectomy.
Hopefully, the demand for evidence based urology treatment will grow, and that lessons have been learned from the way robotic-assisted surgery was introduced. Men with prostate cancer do deserve better.
![]() Kang, D., Hardee, M., Fesperman, S., Stoffs, T., & Dahm, P. (2010). Low Quality of Evidence for Robot-Assisted Laparoscopic Prostatectomy: Results of a Systematic Review of the Published Literature European Urology, 57 (6), 930-937 DOI: 10.1016/j.eururo.2010.01.034
Kang, D., Hardee, M., Fesperman, S., Stoffs, T., & Dahm, P. (2010). Low Quality of Evidence for Robot-Assisted Laparoscopic Prostatectomy: Results of a Systematic Review of the Published Literature European Urology, 57 (6), 930-937 DOI: 10.1016/j.eururo.2010.01.034
Graefen, M. (2010). Low Quality of Evidence for Robot-Assisted Laparoscopic Prostatectomy: A Problem Not Only in the Robotic Literature European Urology, 57 (6), 938-940 DOI: 10.1016/j.eururo.2010.02.004