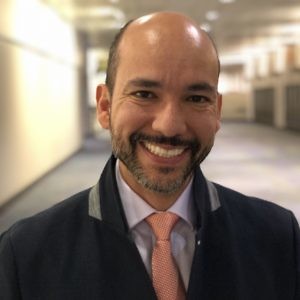
Iraj Ali leads the way at Achilles Therapeutics
There is a lot of interest of late in targeting neoantigens in cancer therapeutically.
At the recent European Society for Medical Oncology (ESMO) meeting, we heard Dr Patrick Ott from the Dana-Farber Cancer Institute present the latest clinical data for Neon’s cancer vaccine approach (See: interview with Dr Ott).
 If you have an interest in neoantigen based cancer treatments, however, then a company on the horizon that we’re excited about is Achilles Therapeutics.
If you have an interest in neoantigen based cancer treatments, however, then a company on the horizon that we’re excited about is Achilles Therapeutics.
It’s an early stage private UK company, in what is very much still a developing and emerging field. Founded just over two years ago, it has a strong academic pedigree. The scientific co-founders are Professors Karl Peggs, Mark Lowdell, Charles Swanton and Sergio Quezada.
BSB readers will recall our prior interviews with Prof Charlie Swanton FRS (See: here and here), where he talked about the groundbreaking TRACERx study he’s leading, some of the insights it is generating regarding neoantigens, and their importance in cancer evolution.
Achilles Therapeutics was established to commercialise the intellectual property being generated from the TRACERx program.
While in London en-route to ESMO18, the CEO of Achilles Therapeutics, Dr Iraj Ali kindly spoke to BSB about where the company is, and some of its future plans.
From what we heard, it’s definitely a company we can expect to hear a lot more about in the cancer immunotherapy space. Check it out!
To learn more from our latest assessment and get a heads up on our oncology insights, subscribers can log-in or you can click to gain access to BSB Premium Content.
This content is restricted to subscribers


 Chicago June 3, 2018: The data for the phase 3 KEYNOTE–042 trial has just been presented in the plenary session of the 2018 annual meeting of the American Society for Clinical Oncology (#ASCO18).
Chicago June 3, 2018: The data for the phase 3 KEYNOTE–042 trial has just been presented in the plenary session of the 2018 annual meeting of the American Society for Clinical Oncology (#ASCO18).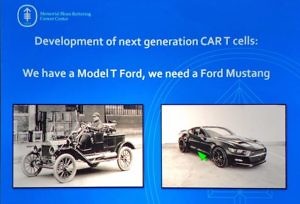 Now that at two CAR T cell therapies have been approved by the FDA in two indications, what does the future hold for new developments in both hematologic malignancies and solid tumours?
Now that at two CAR T cell therapies have been approved by the FDA in two indications, what does the future hold for new developments in both hematologic malignancies and solid tumours?

 There’s a lot of heavy science and jargon inherent in this niche that often frightens off people, but that need not always be the case.
There’s a lot of heavy science and jargon inherent in this niche that often frightens off people, but that need not always be the case.