ASCO21 – we may not be in Chicago, but this year’s virtual ASCO annual meeting does not disappoint in terms of a series of important clinical data emerging, which have the potential to change the cancer treatment landscape.
The results of the Novartis sponsored VISION trial with 177Lu-PSMA–617 in metastatic castration resistant prostate cancer (mCRPC) being presented in Sunday’s plenary session opens the door to a new line of treatment options which can only be of benefit to men with refractory disease.
Whether 177Lu-PSMA–617 will end up being the best radioligand therapy targeting PSMA (Prostate Specific Membrane Antigen) remains to be seen, but the company are to be congratulated in breaking new ground, with a clear path to market strategy enabling them to be the first to market in this indication.
Radioligand therapy combines a radioisotope that causes DNA damage, leading to replication stress or cell death with a tumour targeting compound. It offers a lot of potential in many cancer disease settings and is a topic we expect to hear more about as other companies follow Novartis’ lead and more knowledge is gained about optimal patient selection, dosing, sequencing and combination strategies.

Is it Mardi Gras time at ASCO?
For an expert perspective on what the VISION trial means in the context of the evolving prostate cancer landscape, BSB spoke with Dr Oliver Sartor (Tulane), who participated in the 177Lu-PSMA–617 trial.
Dr Oliver Sartor is a global prostate cancer expert who we’ve had the pleasure to talk with a few times over the years. He’s a professor at Tulane University in New Orleans and Medical Director of the Tulane Cancer Center.
He cheerfully told BSB:
“This is an exciting development with the VISION trial and I think it changes the landscape, even though it is sort of at the end of therapy – these patients were pretty heavily pre-treated.
I think it has implications as we look over the overall landscape for a whole variety of patients, and of course, this therapy is likely to move earlier and trials are already designed to help it move earlier. So I’m excited about the progress for a PSMA targeted therapy with Lutetium–177 and I think it is going to have implications for years to come.”
BSB subscribers can read more of Dr Sartor’s perspective on the VISION trial and emerging prostate cancer landscape, subscribers can log-in or you can click to read our ASCO21 coverage.
This content is restricted to subscribers


 A frequent challenge in oncology R&D is the fast paced nature of pipeline development such that there’s always something cool or new coming along nipping at the heels of those further ahead in clinical development coupled with the changing of the broader landscape before you even get to market.
A frequent challenge in oncology R&D is the fast paced nature of pipeline development such that there’s always something cool or new coming along nipping at the heels of those further ahead in clinical development coupled with the changing of the broader landscape before you even get to market.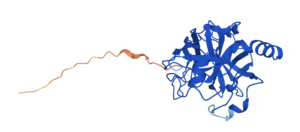

 Resilience in purpose and openess in strategic direction are key dual features in the DNA of strong biotechs which succeed in the long run and live to survive the roller coaster ride that is oncology R&D.
Resilience in purpose and openess in strategic direction are key dual features in the DNA of strong biotechs which succeed in the long run and live to survive the roller coaster ride that is oncology R&D.


